Be yourself; Everyone else is already taken.
— Oscar Wilde.
This is the first post on my new blog. I’m just getting this new blog going, so stay tuned for more. Subscribe below to get notified when I post new updates.
Be yourself; Everyone else is already taken.
— Oscar Wilde.
This is the first post on my new blog. I’m just getting this new blog going, so stay tuned for more. Subscribe below to get notified when I post new updates.
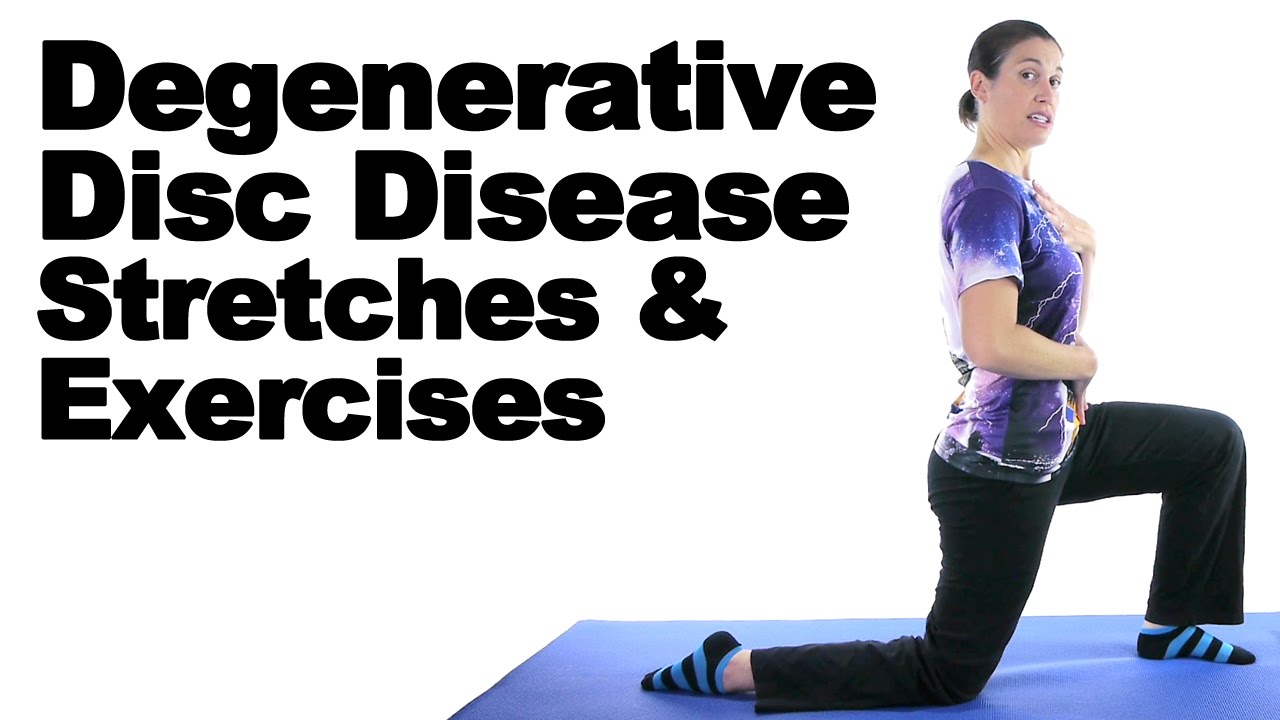
These 4 video low back exercises and stretches may help people with lumbar degenerative disc disease to reduce back pain and build core strength.
| Back Pain Exercise Video: Pelvic Tilt |
| Back Pain Exercise Video: Knee to Chest |
| Back Pain Exercise Video: Lower Trunk Rotation |
| Back Pain Exercise Video: All Fours Opposite Arm and Leg Extension |
The benefits of exercise for lumbar (low back) degenerative disc disease (DDD) are seemingly endless: It strengthens your spinal structures (like bones, muscles, and joints), promotes disc nutrition, and it makes you feel better overall. Your spine specialist may recommend 4 stretches to reduce back pain from low back degenerative disc disease: pelvic tilt, knee to chest, lower trunk rotation, and all fours opposite arm and leg extension.
The exercises and stretches demonstrated in the videos above are designed for people with lumbar DDD. Do you have degenerative disc disease in your neck? Check out Video Series: Exercises for Cervical Spine Degenerative Disc Disease for stretches to incorporate into your fitness routine.
Purpose: To strengthen your lower abdominal muscles and add flexibility to your low back.
How to perform a pelvic tilt:
How can I tell if I’m doing the pelvic tilt right?
Pelvic tilts can help you gently stretch your low back. Photo Source: 123RF.com.
Purpose: To reduce pressure on your lumbar spinal nerves and alleviate back pain.
How to perform a knee to chest:
Alternating knee to chest stretches may help reduce low back pain. Photo Source: 123RF.com.
Purpose: To increase your spine’s mobility and flexibility.
How to perform a lower trunk rotation:
How can I tell if I’m doing the lower trunk rotation exercise correctly?
Modified version of the lower trunk rotation demonstrated in the video. Photo Source: 123RF.com.
Purpose: To strengthen and stabilize your abdominal and low back muscles.
How to perform an all fours opposite arm and leg extension:
Ready to take on an advanced version? If you’re able to comfortably perform this exercise up to 10 times, you may also include your arms in this stretch. Extend your right arm while raising your left leg, and extend your left arm while raising your right leg.
This image demonstrates a modified version of the all fours opposite arm and leg extension exercise that may help you strengthen your abdominal and low back muscles. Photo Source: 123RF.com.
These low-impact exercises focus on strengthening and conditioning your spine’s support system—your core (abdominal muscles) and spinal muscles. What’s the link between a strong core and back health? Your core and spinal muscles act as an internal brace to support your spine. Keeping these structures strong puts less pressure on your spine, so you’ll feel less pain. That’s why exercises designed to strengthen your spine and increase flexibility are so important—stronger spines resist pain.
Staying active also helps keep your discs healthy, as spinal discs need movement for nutrients.
Before starting these stretches or any new exercise program, always talk to your spine specialist first. Low back degenerative disc disease is a condition that warrants extra care before jumping into a new activity, even if it seems as harmless as a gentle stretch. Your doctor’s approval will ensure your activities do what they intend—to help you feel better and not worse.
The 4 stretches described in this article are general guidelines, but your doctor may refer you to a physical therapist or other trainer to show you how to perform other exercises and stretches that take your specific lumbar degenerative disc disease diagnosis into consideration. These professionals may craft an exercise plan for you to help you manage your low back pain and prevent it from worsening.
Finally, remember to take it easy on yourself while exercising. Engaging in low-impact exercises and stretches can make a big difference to the health of your spine. Focus on consistency and listen to your body. If you experience pain or other symptoms (eg, numbness or tingling) during physical activity, stop exercising and call your spine specialist immediately.

If you’ve ever experienced back pain, you are not alone — not by a long shot. “Back pain is one of the most frequent patient conditions we see in healthcare. The vast majority of people will have back pain symptoms at some point,” says Harvey E. Smith, MD, Penn Medicine physician and orthopaedic surgeon. As you get older, your spine ages right along with the rest of you — which can cause disc degeneration. And disc degeneration can lead to back pain. Here are 4 ways this can happen.
In order to understand what happens when you have a herniated disc — and most other back pain caused by disc degeneration— it’s important to first understand the different parts of your spine.
Your spine is made up of bones, called vertebrae, that are stacked on top of one another. Soft, rubbery discs located between the vertebrae act as shock absorbers and provide your back with flexibility. They’re kind of like small, almost-flat water balloons between the bones in your spine. The outside of each disc is made of cartilage. The inside is filled with a jelly-like substance, called nucleus.
These discs can become weakened over time as you age. This can increase the risk of a herniated disc, also called a ruptured disc. When this happens, the jelly-like nucleus substance leaks out into the spinal canal, putting pressure on the nerves. This can cause:
But people of all ages can suffer from a herniated disc. In addition to age-related degeneration, discs can herniate because of:
While herniated discs can be painful, most of the time, they are treatable without surgery. Treatment may include:
In rare cases, surgery to remove all or part of the herniated disc may be necessary.

In addition to vertebrae and discs, your spine also has a spinal cord — a long bundle of nerves — that runs through the center of your vertebrae.
Sometimes the area around the spinal cord narrows. This puts pressure on the cord and nerve roots in the spine.
The most common cause of spinal stenosis is arthritis-related disc degeneration. As the discs degenerate — which also happens as a normal part of aging — the spaces between the vertebrae shrink, which can lead to spinal stenosis.
Symptoms of spinal stenosis include:
Nonsurgical treatment for spinal stenosis is aimed at relieving symptoms and may include:
Surgery is typically only used to treat spinal stenosis that is causing severe pain and weakness. Surgery involves decompressing the spinal nerves by removing nearby bone, bone spurs, and ligaments in a procedure called a laminectomy. In addition to decompression, spinal fusion may also be needed to stabilize the spine.
Sometimes, vertebrae slip forward and out of place. This is called spondylolisthesis. While this can happen because of a broken bone in the back (called spondylitic spondylolisthesis), it is more often caused by the wear and tear that comes with aging (called degenerative spondylolisthesis).
Like spinal stenosis, degenerative spondylolisthesis (DS) can happen because of age or arthritis-related disc degeneration and narrowing of the spinal canal. In fact, spinal stenosis is common in people who have degenerative spondylolisthesis.
Symptoms of degenerative spondylolisthesis include:
The goal of nonsurgical treatment for degenerative spondylolisthesis is symptom relief. This treatment may include:
As with spinal stenosis, surgical treatment involves decompression and spinal fusion and is typically only used when pain and weakness are severe.
While you may be tempted to think of scoliosis as something that only develops during childhood or adolescence, adult-onset scoliosis (called degenerative scoliosis or de novo scoliosis) can also occur because of age-related disc degeneration.
In this case, the spine curves abnormally as the space between the discs collapses.
Symptoms of degenerative scoliosis are similar to symptoms of other degenerative disc diseases, and may include:
Treatment can include:
In severe cases, surgery may be necessary in order to:
No matter the cause of your back pain, Penn Medicine’s Spine Center is ready to help.
“The Spine Center embraces a multidisciplinary team approach to care,” says Dr. Smith. “We introduce you to your care team early on, and are with you through the diagnostic work-up and beyond.
Dr. Smith adds that the multidisciplinary approach allows for providers to collaborate across the different Spine Center specialties and gives patients access to new and innovative treatments and technologies
No matter the cause or course of treatment, the goal in treating back pain caused by age-related disc degeneration is always the same: restoring your quality of life.

Phục hồi chức năng thoái hóa cột sống thắt lưng là điều cần thiết. Những bệnh gây đau lưng nếu như không được chữa trị và phục hồi chức năng, sẽ rất dễ gây ra các biến chứng khôn lường.
Thoái hóa thắt lưng là một bệnh lý mãn tính, thường được phát hiện ở những người trung niên trở nên, nhưng những năm gần đây tỷ lệ người trẻ mắc bệnh có dấu hiệu tăng dần. Bệnh thường có dấu hiệu ban đầu là đau mỏi lưng, nếu bắt gặp tình trạng này, bạn chớ nên coi thường.
Đau thắt lưng là tình trạng đau khu trú, bắt đầu từ khu vực ngang đốt sống ở thắt lưng, xuống các nếp lằn mông. Có thể bắt gặp tình trạng này ở những người lao động, sinh hoạt hàng ngày với điều kiện nặng nhọc.

Có tới trên 65% số người ở lứa tuổi trưởng thành gặp phải vấn đề này, ít nhất một lần trong đời. Đau lưng sẽ ảnh hưởng rất lớn tới đời sống sinh hoạt cũng như lao động của bệnh nhân. Điều này do chính chức năng giải phẫu đặc biệt của vùng thắt lưng, khiến cho vùng cột sống này chịu rất nhiều áp lực, chống chịu toàn bộ sức nặng của cơ thể trong cả ngày làm việc.
Không những thế, thắt lưng là khu vực có tầm vận động rất rộng, bao gồm các động tác, nghiêng mình, cúi mình, ngừa xoay, biên độ vận động cũng khá lớn, được coi là vị trí bản lề đảm nhiệm chính đa số vận động của toàn bộ cơ thể. Ở nước ta, đau thắt lưng chiếm khoảng 2% dân số và 6% trong số tổng các bệnh liên quan tới xương khớp. Đau thắt lưng do thoái hóa cột sống là một vấn đề vô cùng phức tạp, khiến cho người bệnh chịu nhiều tổn thương và đau đớn, có khả năng gây ra nhiều biến chứng nguy hiểm vô cùng.
Để chẩn đoán bệnh, bác sĩ có thể chỉ định người bệnh áp dụng phương pháp chụp X-quang, chụp cộng hưởng MRI, Chụp cắt lớp CT… để có thể tìm kiếm nguyên nhân gây bệnh.
Nếu không được chẩn đoán và điều trị sớm, bệnh có thể phát triển các biến chứng như: Teo cơ, rối loạn cảm giác, rối loạn đại tiểu tiện, lao cột sống, liệt nửa người, liệt toàn thân, gù, gai đôi cột sống, loãng xương…
Ở giai đoạn này, người bệnh buộc phải kết hợp giữa tập các bài vật lý trị liệu, bao gồm: Chườm nóng, điện xung kích thích, dẫn thuốc bằng điện phân và siêu âm trị liệu. Điều này sẽ giúp tăng cường chuyển hóa và chống lại các triệu chứng phù nề, chống viêm cực tốt.
Người bệnh cần tiếp tục chườm nóng, sau đó kích thích điện, siêu âm trị liệu kết hợp với xoa bóp nhẹ nhàng, giúp kéo giãn cột sống vùng thắt lưng, tác động lên các đốt cột sống và tập vận động cho vùng thắt lưng đang bị đau.
Thực hiện bài tập nghiêng xương chậu, tập các nhóm cơ vùng lưng. Người tập bắt đầu với tư thế nằm ngửa, háng gập, tập các bài từ mức độ dễ tới khó. Người bệnh phải để lưng đè xuống mặt giường, hoặc có thể để lưng đè lên tay và đặt ở dưới lưng. Có thể đưa mông lên cao hơn và giũ không cho lưng và mông ưỡn ra phía trước. Tiếp đó người bệnh phải tập tư thế đứng bằng lưng và gót chân.
Tập bài tập làm săn chắc cơ bụng: Người bệnh có thể sử dụng gối và háng để gập lại, cuộn thân vào sao cho mũi có thể chạm vào gối. Tiếp đó có thể tập với tư thế ngồi sang tư thế nắm tay vịn vào hai đầu gối và thả lỏng người ra sau.

Phục hồi chức năng thoái hóa cột sống thắt lưng bằng thuốc: Thuốc giảm đau (acetaminophen), giảm cơn đau và chống viêm (mobic, arcoxia…); glucosamin sulfate hoặc có thể sử dụn glucosamin chondroitin sulfate liều 1500mg/ngày; thuốc làm giãn cơ: myonal 100mg/ngày.
Tài liệu tham khảo:
This is an example post, originally published as part of Blogging University. Enroll in one of our ten programs, and start your blog right.
You’re going to publish a post today. Don’t worry about how your blog looks. Don’t worry if you haven’t given it a name yet, or you’re feeling overwhelmed. Just click the “New Post” button, and tell us why you’re here.
Why do this?
The post can be short or long, a personal intro to your life or a bloggy mission statement, a manifesto for the future or a simple outline of your the types of things you hope to publish.
To help you get started, here are a few questions:
You’re not locked into any of this; one of the wonderful things about blogs is how they constantly evolve as we learn, grow, and interact with one another — but it’s good to know where and why you started, and articulating your goals may just give you a few other post ideas.
Can’t think how to get started? Just write the first thing that pops into your head. Anne Lamott, author of a book on writing we love, says that you need to give yourself permission to write a “crappy first draft”. Anne makes a great point — just start writing, and worry about editing it later.
When you’re ready to publish, give your post three to five tags that describe your blog’s focus — writing, photography, fiction, parenting, food, cars, movies, sports, whatever. These tags will help others who care about your topics find you in the Reader. Make sure one of the tags is “zerotohero,” so other new bloggers can find you, too.